Home Health Medicare News - Recently, the Kaiser Family Foundation has released a new report stating that more than one third of the nation’s 15,500 nursing homes received a rating of 1 to 2 stars under the federal Five-Star Compare ratings system.
The ratings system assigns ratings between 1 to 5 stars to all Medicare and Medicaid-certified nursing homes based on various performance markings in the staffing, inspections, and quality of care.
The reports findings are as follows:
Key Findings
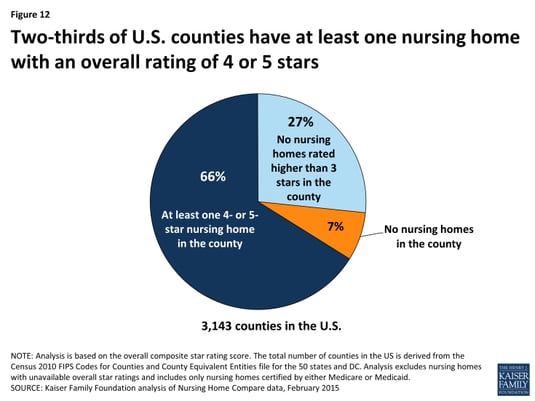
- More than one-third of nursing homes certified by Medicare or Medicaid have relatively low overall star ratings of 1 or 2 stars, accounting for 39 percent of all nursing home residents. Conversely, 45 percent of nursing homes have overall ratings of 4 or 5 stars, accounting for 41 percent of all nursing home residents.
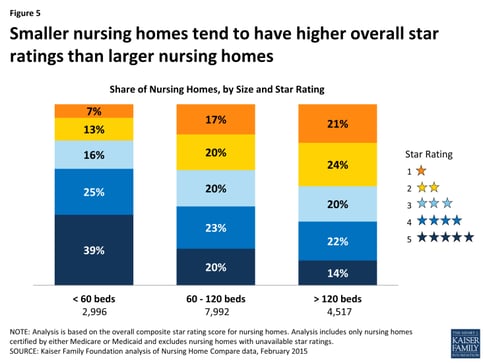
- For-profit nursing homes, which are more prevalent, tend to have lower star ratings than non-profit nursing homes. Smaller nursing homes (with fewer beds) tend to have higher star ratings than larger nursing homes.
- Ratings tend to be higher for measures that are self-reported (quality measures and staffing levels) than for measures derived from state health inspections.
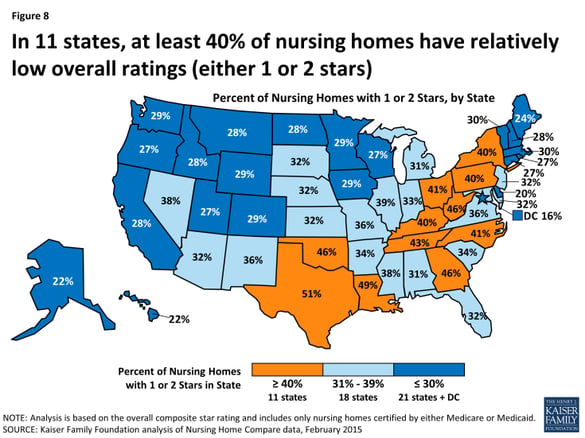
- In 11 states, at least 40 percent of nursing homes in the state have relatively low ratings (1 or 2 stars). In 22 states and the District of Columbia, at least 50 percent of the nursing homes in the state have relatively high overall ratings (4 or 5 stars).
- States that have higher proportions of low-income seniors tend to have lower-rated nursing homes.
Recurrent Problem: Reports of Poor Quality Care in Nursing Homes
Serious concerns about the quality of care in nursing homes have been reported for decades. In 1986, an Institute of Medicine (IOM) report identified several problem areas with nursing home care, including staffing capacity, training, and supervision and made several recommendations regarding oversight and regulation to enhance nursing home standards, particularly those that received federal and state funding. Subsequently, Congress enacted landmark legislation in the Omnibus Budget Reconciliation Act of 1987 (OBRA 87) that, among other provisions, established new minimum requirements for nursing homes eligible to receive Medicare or Medicaid payment, and put in place added enforcement systems. To carry out these provisions, the federal government contracts with states to inspect nursing homes, but states may place additional conditions on nursing homes to meet state licensing requirements. For example, some states require a registered nurse (RN) to be on duty 24 hours a day for nursing homes with 100 or more residents—higher than the federal minimum standard which requires an RN on duty for at least at least 8 consecutive hours per day, 7 days per week, regardless of the number of residents in the nursing home.
In some respects, the quality of care in nursing homes has improved since OBRA 87—such as lower use of physical restraints—but nursing home deficiencies and citations continue to be prevalent. Over the past decade, multiple studies, including those conducted by the Government Accountability Office (GAO) and the HHS Office of the Inspector General (OIG) have found that significant proportions of patients are in nursing homes cited with deficiencies that are serious enough to cause harm or immediate jeopardy. Recent media reports have also described circumstances that raise significant concerns about the quality of care in nursing homes.
Nursing home Compare and the Five-Star Quality Rating System
To help consumers and their families find a nursing home and to encourage nursing homes to achieve higher quality through public reporting of nursing home performance, CMS launched its Nursing Home Compare website in 1998. In 2008, CMS modified the website to provide more user-friendly star ratings based on quality scores for all Medicare- and Medicaid-certified nursing homes. While the ratings provided additional means for consumers to compare nursing homes, some have criticized the heavy reliance on self-reported data. In February 2015, CMS modified its star rating system to begin to address some of these concerns, and is planning additional changes in the future.
The current CMS Five-Star Quality Rating System calculates an overall star rating—with one star being the lowest possible score and five being the highest—based on performance in three types of measures, each of which also has its own five-star rating. These three domains are: 1) state health inspections; 2) staffing ratios; and 3) quality measures. We summarize these domains below and briefly describe how CMS derives a score for each. For more detailed information on the methodology used to calculate individual components and overall quality measures, see Design for Nursing Home Compare Five-Star Quality Rating System: Technical Users’ Guide.
State Health Inspection measures are based on state health inspection reports which provide multiple types of information on nursing home deficiencies identified during annual inspections, including the number and severity of problems, revisits needed to document that deficiencies were corrected, and actions taken by nursing homes to investigate complaints. CMS weights deficiencies that cause “immediate jeopardy to resident health or safety” more heavily when determining each nursing home’s score, particularly when the infractions are widespread and not isolated incidents. Examples of these types of infractions include: failure to prevent or treat residents’ pressure ulcers (bedsores that, if infected, can lead to sepsis and pain); failure to maintain food storage in areas free of pests including rodents and roaches; environmental hazards, such as electrical fires; and failure to follow up on head injuries and fractures among residents.
To help control for variation among states that results from differences in state practices, such as state licensing requirements, the star ratings for State Health Inspections are based on the ranked performance of facilities within a state. That is to say, the star ratings are curved, wherein 5-star ratings are reserved for the 10 percent of nursing homes that received the highest score on the State Health Inspection measure, and 1-star ratings are reserved for the 20 percent of nursing homes that scored the lowest. The remaining 70 percent of nursing homes are evenly assigned 2, 3, and 4 stars. In every state, therefore, 20 percent of nursing homes receive a rating of 1 star.
Staffing measures incorporate information reported by nursing homes on the ratio of nurses to residents, as measured by nurse hours per resident days. This measure adjusts for patient care needs (based on patient acuity levels) at each nursing home and includes calculations of both RN hours per resident days and total nurse hours (including additional types of nurses, such as certified nurse aids) per resident days. To receive a 5-star rating in staffing, a nursing home must have staffing levels that equate to 5 stars for both RNs and total nurses. A nursing home with fewer than 3 hours of total nursing staff per resident days and fewer than 16 minutes of RN time per resident days (both adjusted for patient care needs) would be assigned 1 star in the Staffing star rating.
Quality measures are calculated using the Minimum Data Set (MDS)—an assessment instrument that nursing homes use to document the function and health status of their patients. (The MDS is used for a number of purposes, including determining Medicare payment for patients receiving skilled nursing facility care). Currently, the star ratings incorporate 11 selected measures from the MDS, some of which apply to short-stay patients and the others to long-stay patients. Examples of these measures include the percent of residents with new or worsened pressure sores, the percent of residents who self-report moderate to severe pain, and the percent of residents who experienced falls with major injury. For the total quality score, each of the 11 selected measures is calculated separately to adjust for differences in prevalence, with each measure given equal weight.
Overall star ratings are a composite of the three measure domains, with the State Health Inspection score forming the core of the Overall star rating. Several algorithms apply to the Overall star rating calculation with the general goal of preventing nursing homes from receiving high Overall star ratings if they received low ratings in one or more individual categories. For example, if a nursing home received only 1 star in its State Health Inspection measure, then its maximum Overall star rating is capped at 2 stars. Also, if a nursing home receives only 1 star in the Quality measures category, its Overall rating is reduced by 1 star.
For the full report, visit: http://kff.org/report-section/reading-the-stars-nursing-home-quality-star-ratings-nationally-and-by-state-issue-brief/




