Home health care treatments frequently include invasive devices and procedures to treat patients. Infections can occur from the these procedures/devices, such as catheters, wound care and ventilators.
Healthcare-associated Infections (HAI)
Medicare requires HHAs to monitor for healthcare-associated infections (HAI) as part of its overall Quality Assurance Performance Improvement (QAPI) initiative. Medicare’s Condition of Participation (§484.70 Condition of participation: Infection prevention and control) requires HHAs to “… maintain a coordinated agency-wide program for the surveillance, identification, prevention, control, and investigation of infectious and communicable diseases that is an integral part of the HHA’s quality assessment and performance improvement (QAPI) program."
If your surveillance program yields positive results, i.e. identification of patients with an emerging or active infection, the remedy will include a review of staff and patient training on items such as Standard Precautions and other infection control policies and procedures.
Based on the Center for Disease Control's (CDC) recommendations, your infection SURVEILLANCE should include the following:
1. Monitoring for infection signs and symptoms based on measurable clinical data.
Infection control policies and procedures should include the reporting of potential infection from measurable data collected during routine visits and comprehensive assessments. Some EMRs enable triggering of alerts based on vital signs and symptoms outside of normal parameters. If your EMR does not have this capability, clinical staff will report infection signs and symptoms as part of your incident-reporting system and/or infection-surveillance program.
Infection surveillance definitions require clear, descriptive symptom documentation.
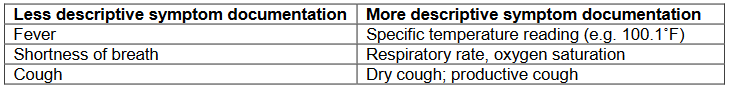
If multiple symptoms are present, the onset date of each symptom should be noted.
Many infection definitions require a change from baseline (e.g. symptom is new or increasing). Consider establishing a protocol for determining and documenting baseline values.
2. Monitoring patients receiving invasive medical procedures
Patients receiving invasive procedures are monitored for emerging infection as part of your infection surveillance activities. The following is a sample list of medical procedures performed routinely in the home setting requiring staff implementation of Standard Precautions. This list is not all-inclusive.
infusion therapy
insertion of and irrigation of nasogatric tubes
insertion of gastrostomy and jejunostomy tubes
tracheostomy care
oral and endotracheal suctioning
chest tube care
inserting and irrigating urinary catheters
CPR
injections
drawing blood
wound care
colostomy/ileostomy care
peritoneal dialysis and hemodialysis
oral hygiene and perineal care
cleaning blood and body fluid spills
washing and changing visibly soiled linens
cleaning medical equipment
transporting lab specimens
handling infectious waste
3. Monitoring patients receiving antibiotics.
Monitoring patients on antibiotics helps to identify
- patients not receiving appropriate antibiotics,
- patients who could have been receiving less expensive antibiotics, and
- patients receiving prolonged antibiotic therapy.
These activities help to reduce antibiotic-resistant pathogen: methicillin-resistant Staphylococcus aureus (MRSA), Clostridium difficile-associated diarrhea (CDAD), and vancomycin-resistant Enterococcus (VRE).
4. Monitoring labwork.
Reviewing the results of all labwork performed on your patient population must also be included as part of infection surveillance.
The following represents lab studies used to identify infection:
- Full blood count —a bacterial infection often raises the white cell count (neutrophilia)
- C-reactive protein (CRP) — elevated above 50 in serious bacterial infections
- Procalcitonin — a marker of generalized sepsis due to bacterial infection
- Rapid Plasma Reagin (RPR) test (and others) — if syphilis is suspected
-
Cultures for throat, urine, sputum, blood, stool and wound
When Healthcare-associated Infections (HAI) are identified in the Home Health Setting
- Report findings to the patient's physician
- Complete an Agency incident report
As part of the Agency's overall Quality Assurance/Performance Improvement (QAPI) Program, agency leaders will evaluate these findings and implement needed changes to employee and patient training, policies and procedures.
-
Authors, F. (1986). Computer Surveillance of Hospital-Acquired Infections and Antibiotic Use. JAMA, 256(8), 1007–1011. https://doi.org/10.1001/jama.1986.03380080053027
-
E.ZoutmanMD, D. (n.d.). The relationship between hospital infection surveillance and control activities and antibiotic-resistant pathogen rates. American Journal of Infection Control, 33(1), 1–5. https://doi.org/10.1016/j.ajic.2004.09.003
-
(n.d.-a). Bacteria Culture Test. Retrieved July 15, 2020, from https://medlineplus.gov/lab-tests/bacteria-culture-test/
-
(n.d.-b). Laboratory tests for bacterial infections | DermNet NZ. Retrieved July 15, 2020, from https://dermnetnz.org/topics/laboratory-tests-for-bacterial-infections/
Does Your Home Health Orientation Include These 11 Policies?
PDGM Therapy: Is PT Always Indicated for a M1860 Mobility Deficit?



