Medicare added the status of a patient's vaccination for influenza (as M1040) in 2009. The answer to "Influenza Vaccine Data Collection Period" (now M1041) is collected at transfer/discharge and discharge but many EMRs - home health software - capture the data on admission, resumption of care and/or recertification. M1041 is also a home health 'COMPARE' question, i.e. a home health agency's Medicare quality ranking is affected by its ability to ensure a patient's protection from the flu...as recorded on its companion question M1046.
Making sure the patient receives a flu vaccination during the flu period (October 1 to March 31)  should be included in the plan of care. Most EMRs enable that functionality - careplanning for a flu vaccine - even though the question is asked at transfer/discharge.
should be included in the plan of care. Most EMRs enable that functionality - careplanning for a flu vaccine - even though the question is asked at transfer/discharge.
These questions determine 1. if the admission is during the flu season (Oct 1 to March 31) and, if yes, did the patient receive a flu vaccine. If not, why did the patient NOT receive the flu vaccine.
M1041, Answered on Transfer or Discharge
Refer only to the most recent SOC or ROC.
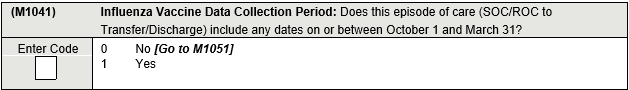
The answer is 'yes' if the patient received any home health services during this 6 month period. If the patient was admitted before the flu season and discharged during the flu season, mark 'Yes'. If the patient was admitted during the flu season and discharged after the flu season, mark 'Yes.
Examples: Patient was admitted on August 15 and discharged on October 2, the answer is is '1 - Yes'.
Patient was admitted on March 15 and discharged on May 1, the answer is is '1 - Yes'.
M1046, Answered if M1041 is 'Yes'
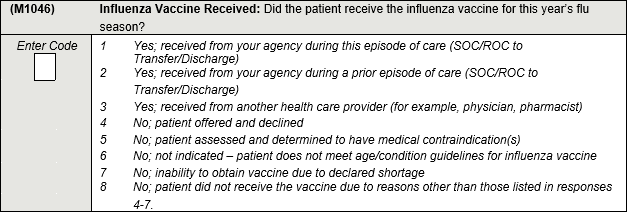
If the Patient DID Receive a Flu Vaccination...Make the Appropriate Selection...
Your agency administered the vaccine during this admission:
1. Vaccine administered during this episode. Enter Response 1 if your agency provided the influenza vaccine to the patient during this episode of care (SOC/ROC to Transfer/Discharge).
2. Vaccine administered during an earlier home health episode by your agency. Enter Response 2 if a current patient was given a flu vaccine by your agency during a previous roster billing situation during this year’s flu season (for example, if the SOC/ROC for this episode was in winter, but your agency provided the vaccine for the current flu season during a previous home health episode in the fall when the vaccine for the current flu season became available).
3. Patient received the vaccine - by someone else - for this year's flu season. Enter Response 3 if the patient or caregiver reports (or there is documentation in the clinical record) that the patient received the influenza vaccine for the current flu season from another provider. The provider can be the patient’s physician, a clinic, or health fair providing influenza vaccines, etc.
Response 1, 2, or 3 may be entered even if the flu vaccine for this year’s influenza season was provided prior to October 1 (that is, flu vaccine was made available early).
If the Patient Did NOT Receive a Flu Vaccine...Make the Appropriate Selection...
4. Patient refused the vaccine. Enter Response 4 if the patient and/or healthcare proxy (for example, someone with power of attorney) refused the vaccine.
5. Vaccine is CONTRAINDICATED for this patient. Enter Response 5 if the influenza vaccine is contraindicated for medical reasons. Refer to the Centers for Disease Control and Prevention (CDC) website for information on contraindications for the influenza vaccine.
Examples include: People who have experienced a severe (life threatening) allergy to a prior dose of a seasonal influenza vaccine (IIV or LAIV); people who have a severe allergy to a component of the IIV vaccine. Health care providers should consult the package inserts for vaccine components.
6. Vaccine is NOT INDICATED for this patient. Enter Response 6 if age/condition guidelines indicate that influenza vaccine is not indicated for this patient. Age/condition guidelines are updated as needed by the CDC. Detailed information regarding current influenza age/condition guidelines is posted to the CDC website. It is the agency’s responsibility to make current guidelines available to clinicians.
Examples include: Infants under the age of 6 months should not receive an influenza vaccine
7. Vaccine is NOT AVAILABLE. Enter Response 7 only in the event that the vaccine is unavailable due to a CDC-declared shortage. Obtain vaccine proof of vaccine shortage: https://www.cdc.gov/vaccines/hcp/clinical-resources/shortages.html
8. Patient did not receive the vaccine for reasons other than above. Enter Response 8 only if the patient did not receive the vaccine due to a reason other than Responses 4–7, including situations where the assessing clinician is unable to determine whether the patient received the influenza vaccination.
Example: patient/family are unreliable in determining if vaccine administered or not. Patient is confused and unreliable. There is no family member able to confirm or deny vaccine administration.
Provide Vaccines Without a Physician Order
Medicare CoPs allow HHA to administer vaccines WITHOUT A PHYSICIAN ORDER.
§484.60(b)(2) Influenza and pneumococcal vaccines may be administered per agency policy developed in consultation with a physician, and after an assessment of the patient to determine for contraindications.
Interpretive Guidelines §484.60(b)(2)
The HHA, in consultation with a physician, must develop a written policy that addresses vaccination screening for safety exclusions and assessing contraindications prior to administration of a vaccine, as well as written policies and procedures that address vaccine administration, including managing adverse reactions. No individual physician order is required for a vaccine. The administration of these vaccines is an exception to
§484.60(b)(1).



