High blood pressure is the most common home health diagnosis.
Home Health Management - High blood pressure is called the “silent killer" because it often has no warning signs or symptoms and patients don't realize they have hypertension. The 'silent' nature of the disease only reinforces the need for patients to regularly monitor their blood pressure, or get blood pressure checked regularly.
The home health clinician's primary role in hypertension care is to educate, give advice, and monitor blood pressure readings. Patient education should focus on modifying behavior related to diet, physical activity, weight, stress, smoking, and alcohol intake
Although the research does not agree about the benefits of nonpharmacological treatment, there are discussions about the extent to which salt restriction and physical activity decrease elevated blood pressure, and the problems h ypertensive patients have coping with salt restriction. To have an effect on blood pressure, weight reduction must be considerable.
ypertensive patients have coping with salt restriction. To have an effect on blood pressure, weight reduction must be considerable.
Conversely, smoking cessation may even increase blood pressure, but the risk of cardiovascular disease from smoking is greater than that from the increased blood pressure after smoking cessation.
Nursing Assessment and Teaching for Hypertension
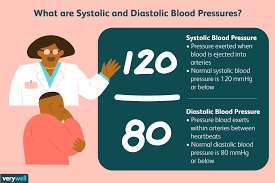
- Record and monitor patient's blood pressure
- Avoid saying “normal” BP, and use the term “well-controlled” to describe patient’s BP within desired limits.
- Assist patient in identifying modifiable risk factors (obesity; diet high in sodium, saturated fats, and cholesterol; sedentary lifestyle; smoking; alcohol intake of more than 2 oz per day on a regular basis; stressful lifestyle).
- Reinforce the importance of adhering to treatment regimen and keeping follow-up appointments.
- Instruct and demonstrate technique of BP self-monitoring. Evaluate patient’s hearing, visual acuity, manual dexterity, and coordination.
- Help patient develop a simple, convenient schedule for taking medications.
- Explain prescribed medications along with their rationale, dosage, expected and adverse side effects, and idiosyncrasies
- Diuretics: Take daily doses (or larger dose) in the early morning;
- Weigh self on a regular schedule and record;
- Avoid or limit alcohol intake;
- Rise slowly from a lying to standing position, sitting for a few minutes before standing. Sleep with the head slightly elevated.
Suggest frequent position changes, leg exercises when lying down. - Recommend
 avoiding hot baths, steam rooms, and saunas, especially with concomitant use of alcoholic beverages.
avoiding hot baths, steam rooms, and saunas, especially with concomitant use of alcoholic beverages.
Instruct patient to consult healthcare provider before taking other prescription or over-the-counter (OTC) medications.
Instruct patient about increasing intake of foods/ fluids high in potassium (oranges, bananas, figs, dates, tomatoes, potatoes, raisins, apricots, Gatorade, and fruit juices and foods/ fluids high in calcium such as low-fat milk, yogurt, or calcium supplements, as indicated). - Encourage patient to establish an individual exercise program incorporating aerobic exercise (walking, swimming) within patient’s capabilities. Stress the importance of avoiding isometric activity.



