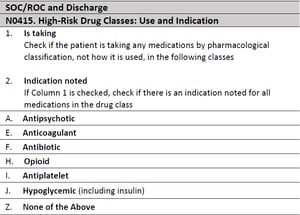
Clinicians are required to teach patients on high risk medications at Start of care and Resumption of Care, per the OASIS question M2010 Patient/Caregiver High-Risk Drug Education. Prior to OASIS-E, Medicare suggested referring to authoritative sources, such as the Institute for Safe Medication Practices, for a list of high risk medications.
Now, on OASIS E, new assessment questions identify the high risk medications on which Medicare wants patients to be taught.
OASIS E finally eliminates the confusion around which high-risk medications require teaching. They are opioids, hypoglycemics, antipsychotics, antiplatelets, antibiotics and anticoagulants.
ANTIPSYCHOTICS
Uses: treatment of psychoses, schizophrenia, schizoaffective disorder, personality disorder and bipolar disorder.
Why they’re a high-risk drug: Common side-effects can be serious, including Parkinson’s-like symptoms, hyperprolactinemia, neuroleptic malignant syndrome, postural hypotension, arrhythmias, sedation, seizures, sexual dysfunction, type 2 diabetes mellitus, anticholinergic effects, dyslipidemia
Specific patient teaching
- Antipsychotics affect people differently.
- Different antipsychotics medications may be prescribed to find the right one that can control symptoms
- Contact the doctor if the medication is not working.
- Don't stop taking antipsychotics suddenly.
- Antipsy
 chotics can interact with other medications. Inform the doctor of all medicines being taken including homeopathic and other over-the-counter medications.
chotics can interact with other medications. Inform the doctor of all medicines being taken including homeopathic and other over-the-counter medications.
Common Antipsychotics: First generation (Typical): Benperidol (Anquil), Chlorpromazine (Largactil), Flupentixol (Depixol), Fluphenazine (Modecate), Haloperidol (Haldol), Levomepromazine (Nozinan), Pericyazine, Perphenazine (Fentazin), Pimozide (Orap), Promazine, Sulpiride (Dolmatil, Sulpor), Trifluoperazine (Stelazine), Zuclopenthixol (Clopixol)
Second generation (Atypical): Amisulpride (Solian), Aripiprazole (Abilify, Abilify Maintena), Clozapine (Clozaril, Denzapine, Zaponex), Risperidone (Risperdal & Risperdal Consta), Olanzapine (Zyprexa), Quetiapine (Seroquel), Paliperidone (Invega, Xeplion)
ANTICOAGULANTS
Uses: Prevention of blood clots.
Why they’re a high-risk drug: Anticoagulants can cause internal bleeding, symptoms of stroke and anemias.
Specific teaching
- Be careful mixing medications. Some antibiotics and anti-fungal medications can make blood thinners more potent and increase the risk of bleeding.
- Tell all health care providers, dentists, physicians, pharmacists that you’re taking blood thinners.
- Always take anticoagulant as directed by the doctor. Don’t skip a dose and don’t double up. If a dose is missed, take it as soon as possible.
- Watch for evidence of internal bleeding. Slow bleeding can cause fatigue, shortness of breath, pale skin color and black, tarry-looking stools. Rapid bleeding can cause stroke symptoms, abdominal and back pain.
- Take precautions to minimize the risk of falls or trauma that could potentially cause significant bleeding.
- Avoid alcohol.
Common Anticoagulants: Apixaban (Eliquis), Dabigatran (Pradaxa), Edoxaban (Savaysa), Enoxaparin (Lovenox), Heparin, Rivaroxaban (Xarelto), Warfarin (Coumadin)
ANTIBIOTICS
Uses: Treatment of bacterial infection
Why they’re a high-risk drug: Frequent and/or inappropriate use of antibiotics can cause bacterial or antibiotic resistance.
Specific teaching
- Take entire prescription; do not stop when feeling "better" as this creates antibiotic resistance.
- Report any adverse response or lack of improvement after 48-72 hr.
There are over 200 unique antibiotics. The most common are: amoxicillin, doxycycline, cephalexin, ciprofloxacin, clindamycin, metronidazole, azithromycin, sulfamethoxazole and trimethoprim, amoxicillin and clavulanate, levofloxacin
OPIOIDS
Uses: Treatment of acute pain
Why they’re a high-risk drug: Opioids are highly addictive, a growing problem throughout the United States. Overdose can cause respiratory depression and death.
Specific teaching
- Opioids are safest when used for three or fewer days to manage acute pain, such as pain that follows surgery or a bone fracture.
- If opioids are needed for acute pain, work with the doctor to take the lowest dose possible, for the shortest time needed, exactly as prescribed.
Common Opioids
- Oxycodone (OxyContin, Oxy, Percocet, Percodan, Roxicet, and Endocet)
- Hydrocodone (Vicodin, Norco, Lortab, Lorcet, and Vicoprofen)
- Codeine (found in combination medicines such as Tylenol #3 or Robitussin AC)
- Hydromorphone (Dilaudid)
- Morphine (MS Contin and Roxanol)
- Fentanyl (Sublimaze, Subsys, Duragesic)
ANTIPLATELETS
Uses: Prevention of blood clots.
Why they’re a high-risk drug: Like anticoagulants, antiplatelets can cause internal bleeding, heavy bleeding or bruising.
Specific Teaching
- Take antiplatelets exactly as prescribed.
- ASA can bother the stomach and should be taken with food. Other antiplatelets can be taken with or without food.
- Do not stop taking antiplatelets unless instructed by the doctor
Common Antiplatelets
- ASA - Acetylsalicylic acid (Aspirin, Asaphen, Entrophen, Novasen)
- Clopidogrel (Plavix)
- Prasugrel (Effient)
- Ticagrelor (Brilinta)
HYPOGLYCEMICS
Uses: Treatment of diabetes
Why they’re a high-risk drug: Hypoglycemics can cause low blood sugar resulting in visual disturbances, loss of consciousness, seizures, death
Specific Teaching
- A meal should be consumed within 30 minutes after administering regular insulin
- Having a strict insulin schedule is essential for keeping blood sugar levels within a healthy range.
- A doctor may prescribe insulins that act at different speeds to keep a person’s blood glucose levels more consistent.
- People at risk of hypoglycemia should wear a medical bracelet stating their type of diabetes, plus other necessary information, such as whether they control their condition with insulin.
- These bracelets provide information to first aiders and medical professionals in case a person becomes conscious.
Hypoglycemics
Oral Hypoglycemic Medications: Sulfonylureas (glipizide, glyburide, gliclazide, glimepiride), Meglitinides (repaglinide and nateglinide), Biguanides (metformin), Thiazolidinediones (rosiglitazone, pioglitazone), α-Glucosidase inhibitors (acarbose, miglitol, voglibose), DPP-4 inhibitors (sitagliptin, saxagliptin, vildagliptin, linagliptin, alogliptin)
Short-acting insulin: regular insulin (Humulin and Novolin)
Rapid-acting insulins: insulin aspart (NovoLog, FlexPen, Fiasp), insulin glulisine (Apidra), insulin lispro (Humalog)
Intermediate-acting insulin: insulin isophane (Humulin N, Novolin N)
Long-acting insulins: insulin degludec (Tresiba), insulin detemir (Levemir), insulin glargine (Lantus), insulin glargine (Toujeo),
Combination insulins: NovoLog Mix 70/30 (insulin aspart protamine-insulin aspart), Humalog Mix 75/25 (insulin lispro protamine-insulin lispro), Humalog Mix 50/5
Antipsychotics: Do they do more harm than good? (n.d.). Retrieved October 28, 2020, from https://www.medicalnewstoday.com/articles/317296
Cherney, K. (2020, June 17). List of Common Diabetes Medications. Retrieved October 28, 2020, from https://www.healthline.com/health/diabetes/medications-list
Insulin therapy: Side effects, myths, and tips. (n.d.). Retrieved October 28, 2020, from https://www.medicalnewstoday.com/articles/323387
Omudhome Ogbru, P. (2019, October 28). Insulin for Diabetes Treatment: Facts about Side Effects. Retrieved
October 28, 2020, from https://www.medicinenet.com/insulin_for_diabetes_treatment_types_side_effects/article.htm
Treatment. (n.d.). Retrieved October 28, 2020, from https://www.rchsd.org/health-articles/the-danger-of-antibiotic-overuse/



