The draft version of the new OASIS-E Start of Care OASIS assessment has fifteen (15) sections. Many of the 'old' questions remain - like M1610 Urinary Incontinence/Catheter Presence. This question is now located under Section H 'Bladder & Bowel'.
- A - Administrative Information
- B - Hearing, Speech, and Vision
- C - Cognitive Patterns
- D - Mood
- E - Behavior
- F - Preferences for Customary Routine Activities
- G - Functional Status
- GG - Functional Abilities and Goals
 H - Bladder and Bowel
H - Bladder and Bowel- I - Active Diagnoses
- J - Health Conditions
- K - Swallowing/Nutritional Status
- M - Skin Conditions
- N - Medications
- O - Special Treatment, Procedures, and Programs
Include the following policies and procedures for documenting OASIS M1610 Urinary Incontinence/Catheter Presence (adapted from OASIS/ICD10 Guidance Manual):
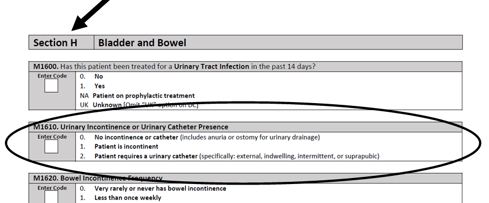
(M1610) Urinary Incontinence or Urinary
Catheter Presence:
- 0 - No incontinence or catheter (includes anuria or ostomy for urinary drainage) [Go to M1620]
- 1 - Patient is incontinent
- 2 - Patient requires a urinary catheter (specifically: external, indwelling, intermittent, or suprapubic) [Go to M1620 ]
Remember…
This question identifies the presence of urinary incontinence or condition that requires urinary catheterization of any type, including intermittent or indwelling. The etiology (cause) of incontinence is not addressed in this item.
Instructions For Assessment
• Select Response 0 if the patient has anuria or an ostomy for urinary drainage (for example, an ileal conduit), or if the patient has a urinary diversion that is pouched (ileal conduit, urostomy, ureterostomy, nephrostomy), with or without a stoma
• Select Response 1 if the patient is incontinent at any time (including “occasionally,” “only when I sneeze,” “sometimes I leak a little bit,” etc.).
• Select Response 1 if the patient is incontinent or is dependent on a timed-voiding program. Timed voiding is defined as scheduled toileting assistance or prompted voiding to manage incontinence based on identified patterns. Time voiding is a compensatory strategy; it does not cure incontinence.
• Select Response 2 if a catheter or tube is utilized for drainage (even if catheterizations are intermittent).
• Select Response 2 if the patient requires the use of a catheter for urinary drainage for any reason (for example, retention, post-surgery, incontinence). Select Response 2 and follow the skip pattern if the patient is both incontinent and requires a urinary catheter.
• Select Response 2 if a catheter was inserted during the comprehensive assessment.
Assessment Strategies
- A leaking urinary drainage appliance is not incontinence.
- A catheter solely utilized for irrigation of the bladder or installation with an antibiotic is not reported in this item.
- If a catheter was discontinued during the comprehensive assessment or if a catheter is both inserted and discontinued during the comprehensive assessment, Response 0 or 1 would be appropriate, depending on whether or not the patient is continent.
 Review the urinary elimination pattern as you take the health history. Does the patient admit having difficulty controlling the urine, or is he/she embarrassed about needing to wear a pad so as not to wet on clothing? Do you have orders to change a catheter? Is your stroke patient using an external catheter? Be alert for an odor of urine, which might indicate there is a problem with bladder sphincter control. If the patient receives aide services for bathing and/or dressing, ask for input from the aide (at follow-up assessment). This information can then be discussed with the patient. Urinary incontinence may result from multiple causes, including physiologic reasons, cognitive reasons.
Review the urinary elimination pattern as you take the health history. Does the patient admit having difficulty controlling the urine, or is he/she embarrassed about needing to wear a pad so as not to wet on clothing? Do you have orders to change a catheter? Is your stroke patient using an external catheter? Be alert for an odor of urine, which might indicate there is a problem with bladder sphincter control. If the patient receives aide services for bathing and/or dressing, ask for input from the aide (at follow-up assessment). This information can then be discussed with the patient. Urinary incontinence may result from multiple causes, including physiologic reasons, cognitive reasons.
Does Your Home Health Orientation Include These 11 Policies?



