A Beginner's Guide to Home Health Billing
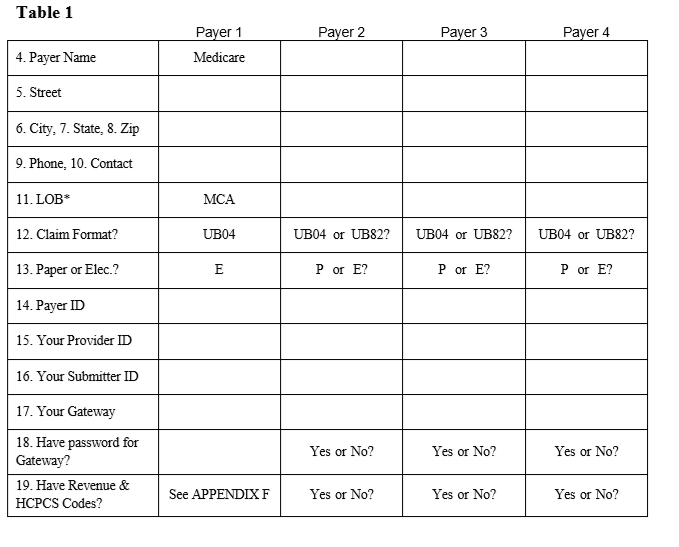
Home Health billing is full of detail and can be frustrating. Submitting claims to different payers takes ALOT of time because each payer has lots of rules and terms for which - for a new home health biller - will be unfamiliar. Your software will only HELP you submit claims but you...
PDGM Home Health Billing: Significant Change in Condition (SCIC)
The home health conditions of participation (CoPs) require that agencies update and revise the current OASIS assessment under the following conditions:
(1) The last 5 days of every 60 days if the patient is to be 're-certified', unless there is a beneficiary-elected transfer,
(2) a...
How to Get a Prior Authorization for Home Health Billing
Certain payers require prior authorizations.
Depending on the payer, a home health agency (HHA) may be required to obtain a ‘prior authorization’ (PA) for home health billing and to determine insurance eligibility. Think of prior authorization as “permission” to provide a type of...
Medicare Home Health Billing: A RAP is Just a Loan
I am constantly surprised at how many agencies authorize RAP after RAP (Request for Advance Payment) and seem to forget about the final claim. It’s great to get that advance payment and use it as Medicare intended...to keep your agency humming along until the final payment is received....
Are Your Physicians Billing Home Health Claims for CPO?
'Care Plan Oversight' can earn physicians thousands per month. Provide the following guidance to physicians to enhance your referral-building relationships.
adapted from the Medicare Learning Series: Care Plan Oversight Home Health (CPO) is physician supervision of patients under...
Denial of Home Health Payments When OASIS Not Received
Medicare Change Request (CR) 9585 directs Intermediaries to automate the denial of Home Health Care Billing Prospective Payment System (HH PPS) claims when the condition of payment for submitting patient assessment data has not been met. Make sure that your HH billing software staff...
Medicare is on Warpath for Never-Ending Home Health Recertifications
LAZINESS OR NECESSITY? It’s pretty easy to keep a patient around by sending in a nurse to administer a B12 shot or take vital signs once a week, or perhaps by throwing in an occasional PT visit for home health billing. I’ve watched several agencies recertify patients not just month...